“Variola” may not sound like an intimidating name, but throughout history there was no name more feared. Daniel Koplow in his book, Smallpox: the Fight to Eradicate a Global Scourge, says about variola (better known to English speakers as smallpox), “Over a period of at least three millenia it was second to none in inflicting human pain, suffering and death. By some estimates, smallpox killed as many as 500 million people during the twentieth century alone.”1 Allan Chase agrees, calling smallpox “the worst pestilence ever to afflict mankind.”2 Once the reigning king, this virus has now been consigned to less than 600 samples in two laboratories on this planet and may eventually be condemned to intentional extinction. If nothing else, variola has a unique place in history.
The origin of the virus is unknown, but many who were smitten by it are not: Ramses V of Egypt (whose mummy bears the characteristic scarring of a smallpox victim), Elizabeth I of England, George Washington, as well as billions of people whose names never made it into the annals of history. The symptoms were obvious and the scars unmistakable. After around two weeks of incubation, it might feel like the flu with fever and aches, but a very few days later an unmistakable crop of “postules” (raised bumps under the skin that were hard to the touch) formed and inflicted more pain and discomfort on the sufferer for another couple of weeks. Many of the postules left unsightly scars on the face, neck, and extremities. No one who got the disease escaped without some scars. No one knew how to cure it. No one who was fortunate enough to survive it ever came down with it again.
Many doctors in many cultures had their methods of preventing it, but one method that seemed to work arose in the Asian and African cultures centuries before it was used in the West. These cultures discovered that induced cases were rarely as vicious as naturally acquired smallpox, and they also had a low fatality rate (1% compared with the naturally-occurring case rate of 30%). When it was introduced to the West, it was called “variolation” or “inoculation,” and it was greeted with suspicion and distrust. Westerners often chose not to practice it for several reasons, not the least of them being that it was still considered unsafe by many doctors. Since patients were typically given the disease through contact with an infected person’s blood or lymph, sometimes other diseases such as hepatitis and syphilis were passed on with it, causing severe complications.3 Also, during the course of their inoculation, patients could pass along full-blown cases of smallpox to their loved ones, so they had to be kept in strict quarantine, a measure that was not always successful. Still, it was used with much success in many cultures and was eventually adopted by many European countries and mandated by George Washington for the Continental Army in 1777.4
Many in the New England colonies viewed this practice as evil to the core. Writing in the 18th century, John Williams said, “I do seriously believe it’s a delusion of the Devil; and that there was never the like delusion in New-England since the time of the witchcraft at Salem.”5 Samuel Grainger wrote a letter to a friend attempting to dissuade him from accepting the practice and appealed to a variety of arguments. Hoping most of all to base his viewpoint on the Bible, he believed that smallpox was judgment from God, either for personal or national sin. He felt that the only means available afforded by the Bible for dealing with a pestilential disease was to repent of sin and reform one’s ways. Circumventing judgment by taking steps to prevent the disease only brought on further judgment from God. “Must the Supreme Providential Will become subservient to the becks and appointment of the human will, or must the human will say, the divine will be done,” he wrote6 . The fact that a person undergoing inoculation could pass along smallpox to his neighbors bothered him as well since we are commanded by the Bible to love our neighbors7.
Others defended the practice against these arguments with varying degrees of success. William Cooper wrote in 1721, “To bring sickness upon oneself for its own sake, is what no man in his right wits would do. But to make myself sick in such a way, as may probably serve my health, and save my life, and with such a design is certainly fitting and reasonable and therefore lawful.”8 Eventually, the attitude of another writer, James Jurin, put the controversy over inoculation in a striking light, “He [any physician] will consider, whether it will be for his reputation, where his friend and his patient shall put his life, or the lives of his children, into his hands, to amuse himself with theological disputes and scruples, whether it be lawful to save them. For if the practice of inoculation be really found to be a means of preserving life, it will not be easy to make the world believe, that it is criminal to use it.”9
It took a middle-aged country doctor in England to bring the king of infectious diseases to it knees. Edward Jenner of Berkeley, Glouchestershire had treated many patients throughout his medical career, and he would often treat sufferers of a disease called cowpox. Although it afflicted cows primarily, many milkmaids would contract the disease from the cows they milked. It always had more benign (although similar) manifestations than smallpox, and it was a well-known proverb of the milkmaids that those who got cowpox never got smallpox. Curious, Dr. Jenner, who had been variolated as a boy and therefore could not test it out on himself, took some lymph from a milkmaid’s infected hand and infected eight-year-old James Phipps with it on May 14th of 1796. In early July, he injected James with smallpox and waited. Nothing happened. He tried again a couple of weeks later, but the boy was immune to the virus. Jenner surmised that cowpox was related to smallpox and provides crossimmunity, that is, immunity against both itself and its related viruses, to the person who recovers from it. He called his process “vaccination” from the Latin word “vacca” or “cow.” The medical fields of vaccination and immunology developed out of that single discovery – and so did the death of smallpox.10
The news of Jenner’s discovery swept Europe where, for instance, Bavaria made obligatory vaccination the law in 180711. Many nations’ militaries followed suit, though the nations themselves did not because of many who mistrusted the practice. Vaccination was much less expensive than variolation. Beyond being safer for the patients, it was much cheaper and safer for others around them than variolation. Some practitioners of variolation were displeased with these advantages because they were bad for business, and vaccination did not earn as much for them. Some doctors honestly feared for the safety of those being vaccinated because of the rare side effects or complications from the procedure. Others who were heavily involved in the sanitation and public reform movements thought that smallpox could be controlled by increased sanitation, thus making vaccination unnecessary. Still others, like Reverend Thomas Robert Malthus, thought that smallpox was God’s means of keeping the unworthy poor from overrunning the earth’s population, and thus it should not be diminished by such measures.12
Slowly the method of vaccination was refined. It must be remembered that vaccination was invented and implemented long before any nation had strict controls on medical products and procedures. Also, the workings of the disease and of the human immune system were largely unknown when this practice was discovered, thus making true knowledge of how to improve it much more difficult. For many patients early on, the process was done by arm-to-arm contact, but this brought with it the same risks of contamination for other diseases, such as hepatitis and syphilis, that inoculation had13. Soon the vaccine was taken from bovine sources instead to prevent contamination. When it was discovered that glycerin inhibited the propagation of all kinds of bacteria, it was added to vaccines in order to prevent many bacterial contaminants.14 The current vaccine stocked by the World Health Organization is made from “pulp scraped from vaccine-infected animal skin, mainly calf and sheep, with phenol added to a concentration sufficient to kill bacteria but not so high as to inactivate the vaccinia virus.”
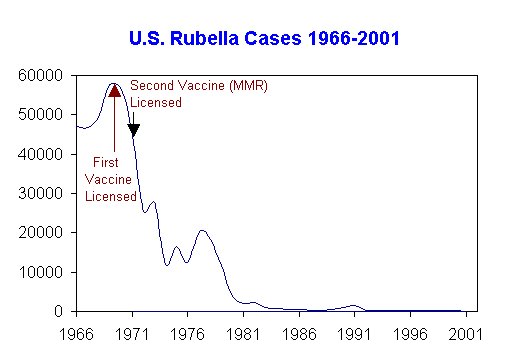
With aggressive use, the vaccine quickly tapered off the number of cases throughout the world. In 1948, the United Nations created the World Health Organization (WHO). Early on, it focused its attention on smallpox. Global involvement was considered key in the process of fully stopping this dread disease – as long as there was one place where the virus lived on, anyone who traveled there would be at risk and large- scale vaccination programs would have to continue indefinitely. However, if there were a means of controlling and eventually wiping out the virus’ potential hosts all over the world, humanity could perhaps rest easy at last.
Daniel Koplow points out the wisdom of the coordinators of this effort. Instead of attempting to vaccinate every single person on the globe, the strategy involved quick identification of outbreak sites and vaccination in those immediate areas to prevent further spread. Three things about the nature of the disease aided the eradication campaign. First, everyone who had the virus showed outward signs, making it easier to find outbreaks of the virus. Second, the virus has no non-human carriers, so only where human beings were stricken with it could they find the virus. Also, they did not have to worry about fleas, rats, or other animals carrying it, as happened with the bubonic plague. Third, many nations instituted obligatory vaccination programs for their citizens thus doing the work for the WHO volunteers. Efforts were astonishingly successful in places like West Africa, one of the hotbeds of smallpox in the world, which was declared to be completely free of smallpox within less than four years after the campaign’s work began there15. The last case of naturally-occurring smallpox was found in Somalia in 1979. Aaron Chase adds “The total cost to all the world’s nations of the World Health Organization smallpox eradication program came to only 300 million, or far less than the going price of a half-dozen F-16 or equivalent fighter-bombers.”16 It took a great deal of global coordination, trial and error, and scientific exploration to beat smallpox, but vaccination – the most inexpensive and safe of all medical procedures – made it possible.
References
1. Daniel A. Koplow Smallpox: the Fight to Eradicate a Global Scourge University of California Press, Berkeley, CA 2003, p. 1
2. Allan Chase Magic Shots: a Human and Scientific Account of the Long and Continuing Struggle to Eradicate Infectious Diseases by Vaccination, William Morrow and Company, New York, NY, 1982, p. 51
3. Ibid., p. 74
4. Daniel A. Koplow, p.18
5. John Williams “An Answer to a Late Pamphlet, intitled, ‘A Letter to a Friend in the Country, Attempting a Solution of the Scruples and Objections of a Consciencious or Religious Nature, Commonly Made Against the New Way of Receiving the Smallpox’ ” Early American Imprints. First Series, no. 2407 Readex Microprint (New York), 1985, p. 4
6. Samuel Grainger “The Imposition of Inoculation as a Duty Religiously Considered in a Leter[sic] to a Gentleman in the Country inclin’d to Admit It” Early American Imprints. First Series, no. 2222 Readex Microprint (New York), 1985, p.12
7. Ibid., p.25
8. William Cooper “A Letter to a Friend in the Country, Attempting a Solution of the Scruples and Objections of a Conscientious or Religious Nature, Commonly Made Against the New Way of Receiving the Small-pox.” Early American Imprints. First Series, no. 2247 Readex Microprint (New York), 1985, p.3
9. James Jurin An Account of the Success of Inoculation the Small Pox in Great Britain: with a Comparison but MisCarriages in that Practice, and the Mortality of the Natural Small-pox 2nd edition. Printed for J. Peele (London), 1724, p. 4
10. Allan Chase, p. 42-46
11. Ibid. p. 62
12. Ibid. p. 72-3
13. Daniel Hopkins The Greatest Killer: Smallpox in History, with a New Introduction University of Chicago Press (Chicago), 2002, p. 85
14. Fenner, F. Smallpox and its Eradication World Health Organization, (Genva) 1988 ( Available online)
15. Ibid. p. 23
16. Ibid. p. 82
Erica A. Sommerville is not a medical doctor but a college student. She does not dispense medical advice. Her aim is to educate the public about scientific issues. Please consult a board-certified medical doctor before making any medical decisions for yourself or your family.