(click for credit)
Approximately a year ago, I wrote about the bacteria in human breast milk. While that may sound like a bad thing, it is actually a very good thing. Over the years, scientists have begun to realize just how important the bacteria that live in and on our bodies are (see here, here, here, here, and here), and the bacteria in breast milk allow an infant to be populated with these beneficial microbes as early as possible. Not surprisingly, as scientists have continued to study breast milk, they have been amazed at just how much of it is devoted to establishing a good relationship between these bacteria and the infant who is consuming the milk.
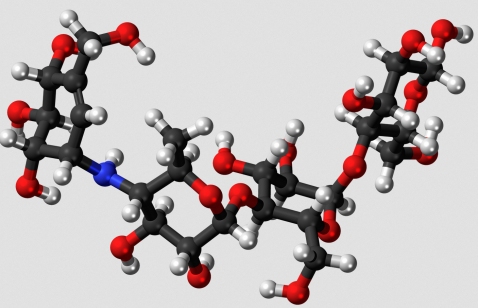
For example, research over the years has shown that human breast milk contains chemicals called oligosaccharides. These molecules, such as the one pictured above, contain a small number (usually 3-9) simple sugars strung together. Because oligosaccharides are composed of sugars, you might think they are there to feed the baby who is consuming the milk, but that’s not correct. The baby doesn’t have the enzymes necessary to digest them. So what are they there for? According to a review article in Science News:1
These oligosaccharides serve as sustenance for an elite class of microbes known to promote a healthy gut, while less desirable bacteria lack the machinery needed to digest them.
In the end, then, breast milk doesn’t just give a baby the bacteria he or she needs. It also includes nutrition that can be used only by those bacteria, so as to encourage them to stay with the baby! Indeed, this was recently demonstrated in a study in which the authors spiked either infant formula or bottled breast milk with two strains of beneficial bacteria. After observing the premature babies who received the concoctions for several weeks, they found that the ones who had been feed bacteria-spiked formula did not have nearly as many of the beneficial microbes in their intestines as those who had been feed bacteria-spiked breast milk.2
But it turns out that these oligosaccharides do more than just feed the desirable microbes; they also repel the undesirable ones! In a review article written for the journal Glycobiology, Lars Bode calls them Human Milk Oligosaccharides (HMOs). He says:3
An accumulating body of evidence suggests that HMOs are antiadhesive antimicrobials that serve as soluble decoy receptors, prevent pathogen attachment to infant mucosal surfaces and lower the risk for viral, bacterial and protozoan parasite infections.
So if these HMOs are so beneficial to children, shouldn’t scientists be trying to put them in infant formula for those babies who cannot be breastfed? That would be ideal, but as the Science News article I mentioned puts it:4
But extracting or producing human milk oligosaccharides on an affordable, industrial scale won’t be easy. Synthesizing the sugars is an expensive headache because the molecules – about 200 of which have been identified so far – are put together in a dizzying array of configurations.
In the end, the most likely alternative for getting them into infant formula is to genetically engineer some bacteria to produce the most useful ones for us.
When I was born, it was popular to avoid breastfeeding so mothers could use a “scientifically-developed” infant formula. Some people actually thought that scientists could design a better food for babies than what was found in breast milk. Of course, if breast milk had been produced by random mutation filtered through natural selection, that would probably have been true. However, breast milk has been designed by an all-powerful Creator to provide infants with just what they need. As current research clearly shows us, it is significantly better than anything that can be designed by even our best scientific endeavors.
REFERENCES
1. Jessica Shugart, “Motherlode: Superhero sugars in breast milk make the newborn gut safe for beneficial bacteria,” Science News January 11, 2014, p. 22
Return to Text
2. Underwood MA, Kalanetra KM, Bokulich NA, Lewis ZT, Mirmiran M, Tancredi DJ, and Mills DA, “A comparison of two probiotic strains of bifidobacteria in premature infants,” Journal of Pediatrics 163:1585-1591.e9, 2013 (Please note that the decision to feed the children formula or bottled breast milk was not associated with the study in any way.)
Return to Text
3. Bode, L, “Human milk oligosaccharides: every baby needs a sugar mama,” Glycobiology 22:1147-62, 2012
Return to Text
4. Jessica Shugart, p. 23
Return to Text
What a great article to encourage young woman to breastfeed! Thank you for writing it.
I always love your articles
Dr. Wile,
I have to take exception to your last paragraph. While I agree with you that the evidence has shown mother’s milk is far superior to that which is man-made, your assertion that: “if breast milk had been produced by random mutation filtered through natural selection, that would probably have been true” is lacking in the evidence that I find you usually provide. While I understand the creation over evolution bias as the basis for the baseless assertion, you have historically backed up your assertions with evidence.
It is my understanding that the theory of evolution doesn’t ascribe random chance as the method things last and remain in populations, but rather selection for increased survival rates. That is, if a beneficial relationship developed between the oligosaccharides and bacteria mentioned above, and it provided a survival benefit to the hosts of that strain, those hosts would have a better chance of surviving and therefore would reproduce and pass along that advantage. This finding does nothing to weaken the theory of evolution, if anything it fits rather nicely.
I would agree with you that it speaks strongly to the benefits of breast feeding over not, but once the hubris of 60’s and 70’s formula makers failed under the evidence gathered, we had pretty much come to that conclusion anyway. It is just nice to know more reasons what that is so. Yet another benefit of following the evidence.
Thanks for your comment, Jase, but I will have to disagree with you. The description I gave is exactly what the hypothesis of evolution says. Mutations are random. There is no goal in mind. If those mutations provide some survival benefit, they are selected. That’s why I said “random mutation filtered through natural selection.” Neo-Darwinism says that the basis of evolution is random, and that random change is then filtered through natural selection to produce evolution.
In the case of breast milk, this scenario is dubious, at best. For example, the relationship upon which natural selection is acting is not the relationship between the oligosaccharides and the bacteria. It is the relationship between the breast milk and the infant. The mother is the one who makes the oligosaccharides. In order to explain this in the context of the hypothesis of evolution, you need to explain how the mother developed genes for producing those oligosaccharides, despite the fact that humans have no use for them. Also, you have to explain how the regulatory apparatus developed to make sure that the oligosaccharides found their way only into breast milk. In addition, you have to explain how they just happen to be the right oligosaccharides for the beneficial bacteria and not the ones that would nourish the pathogenic bacteria. Thus, this finding doesn’t fit nicely with the hypothesis at all. Instead, it produces several hurdles that the hypothesis will have a hard time overcoming. However, it does fit very nicely with the idea that God designed breast milk.